Inflammation of the prostate today is the leader in the group of male diseases, transmitted mainly through sexual contact. Its complications threaten infertility, decreased libido, impotence.
The first symptoms of prostatitis in men
Prostatitis is an inflammatory disease. This is one of the most common urological pathologies, which is diagnosed in representatives of the strong half of humanity.
Most often, this anomaly is detected in men over the age of thirty, although recently the disease has become much younger. Treatment of prostatitis should be carried out by qualified specialists (urologists or andrologists), since there is a high probability of developing various kinds of complications.
How is prostatitis treated?
With the help of drugs
- NSAIDs - relieve inflammation, fever and fever. They have a slight analgesic effect. With the onset of prostatitis, a short treatment with anti-inflammatory drugs and taking vitamins is required to maintain the gland in a normal state. Men are prescribed: Diclofenac, Nise, Voltaren, Nimesulide. The drugs are produced in suppositories, tablets, injections.
- Antibiotics - designed to eliminate the infectious or bacteriological factor of inflammation. The treatment regimen for prostatitis is signed after the pathogen has been identified and its resistance to antibiotics has been tested. The course of treatment is 7-10 days. In severe cases, therapy is extended up to two weeks.
- Hormones are recommended if the usual course of medications has not been beneficial, as well as with a decrease in sexual desire due to advanced disease. Treat with hormones at an early stage is prohibited. The drugs are taken under the strict supervision of a urologist.
- Symptomatic drugs - to eliminate the pain syndrome, take Aspirin tablets. Spasms are removed by No-shpa. With persistent intense pain, blockade with Novocain is indicated.
- Vitamins and medicines to keep the prostate functions in working order. During the period of remission, it is recommended to drink drugs to normalize metabolism and improve blood supply to glandular tissues, and juice production. For this, phytopreparations are prescribed: Prostamol-Uno, Prostate-forte and the like. To strengthen the immune system, a complex of vitamins and minerals is shown: Duovit, Vitrum.
Self-medication is dangerous, it does more harm than good. Before taking any of these drugs, you need to consult a urologist.
With the use of physiotherapy
- UHF and microwave.
- Magnetotherapy.
- Mud cure.
- Galvanization.
- Ultraphonophoresis.
- Laser treatment.
- Heat therapy.
natural remedies
Diagnostics
To start the treatment of inflammation of the prostate on time, you need to contact a competent specialist who will conduct a comprehensive examination and make the correct diagnosis. The list of recommended diagnostic methods includes the following:
- Blood tests - conduct a study of the biochemical composition, for the content of PSA (prostate-specific antigen), general analysis and PCR if necessary.
- Urinalysis - the man is asked to urinate in several different containers in order to conduct the study in different ways.
- Scraping from the surface of the urethral canal to detect an infectious pathogen.
- Bacteriological culture of prostate secretion and urethral secretions to determine the bacterial pathogen and its resistance to medications.
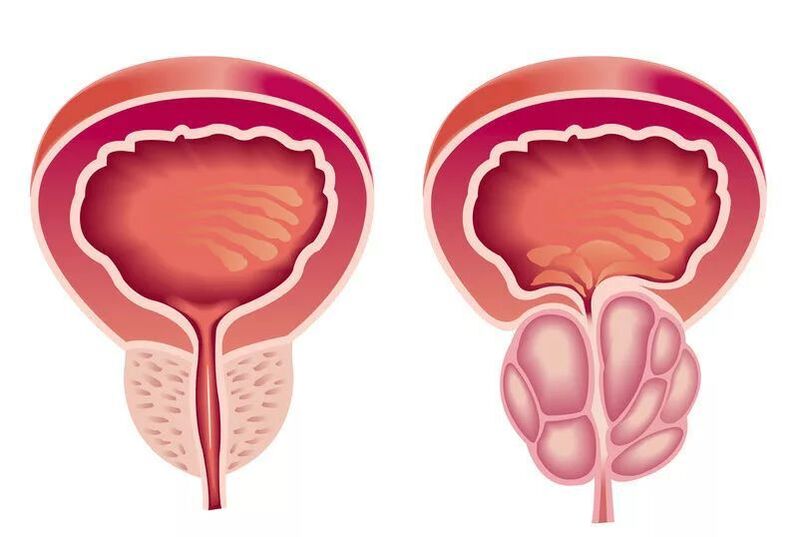
- Ultrasound of the prostate - allows you to assess the size and shape of the gland, the presence or absence of fusion of tissues, adhesions and cicatricial changes.
A mandatory item in the diagnosis of prostatitis is a rectal digital examination. Finger examination allows the doctor to feel the gland and evaluate its density, structure, shape and size. Also, during a rectal examination, a secret of the prostate is obtained, which is then sent for analysis. Additional examination methods are assigned to a particular patient individually if indicated.
These can be measurements of urine flow velocity, magnetic resonance or computed tomography, x-rays of the pelvic organs, and other methods.
Acute prostatitis
The disease begins with a sharp rise in temperature (up to 40 degrees), excruciating headache, fever. The symptoms that appear are accompanied by pain in the groin, perineum, back, discharge from the urethra, frequent urination and constant urge to urinate.
The emptying of the bladder occurs with a delay, a burning sensation. The urine itself becomes cloudy, and an admixture of blood may appear in it. There is irritability, fatigue.
The outcome of acute prostatitis can be a complete resolution of the process (with timely treatment). Since changes occur in many organs of the small pelvis, they cannot be left to chance, otherwise the corresponding complications will arise:
- Vesiculitis is an inflammation of the seminal vesicles, the cause of pus in the semen, which not only reduces the quality of the ejaculate, but leads to a loss of reproductive function.
- Colliculitis - inflammatory changes in the seminal tubercle become the reason for the development of severe pain during sex, interruption of orgasm, impotence of a psychological nature.
- The formation of an abscess in the body of the prostate, its rupture, purulent damage to the rectum leads to an exacerbation of symptoms, a powerful intoxication of the body, up to death.
- Stagnation in the tissues of the prostate leads to a change in their structure, disruption of innervation, blood supply, both to the gland itself and to organs located nearby, with a violation of their functions. The erection becomes insufficient for a full-fledged sexual intercourse, premature ejaculation is observed, prolonged sexual intercourse without the onset of orgasm.
- Cicatricial changes in the gland, spermatic cord lead to infertility, a decrease in the qualitative composition of sperm, and sperm motility. Narrowing of the urethra interferes with the normal process of urination, bladder obstruction can cause acute urinary retention, requiring emergency surgical care.
Main symptoms
As noted above, the disease can be chronic and acute. A common and one of the most important symptoms is increased urination. A healthy man usually experiences no more than 10-11 urges to urinate during the day (the normal figure is 5-6 urges).
As a result of the development of inflammation of the prostate, a negative effect on the bladder occurs, therefore, in the presence of the disease, the following symptoms will appear:
- An increase in the number of urges (while the daily volume of urine remains the same).
- Urine comes out in small portions, which is associated with receiving false signals from the bladder receptors due to the presence of an inflammatory process. Also, therefore, there may be a feeling that the bladder is full even after emptying.
- Pain during urination, which is due to the narrowing of the urethra due to the inflammatory process in the prostate.
- Difficulty urinating due to compression of certain areas of the urethra by inflammation. In some cases, men cannot empty their bladders at all because of this.
- At night, the walls of the bladder begin to give false signals, which increases the number of trips to the toilet during sleep.

Part of the diagnosis of prostatitis can also be made by monitoring body temperature, coupled with problems associated with urination. If these problems are accompanied by an increase in temperature to subfebrile and febrile values, then it is possible to speak with a high degree of probability of the development of pathology. It is important to note that in the later stages of the development of the disease, on the contrary, a decrease in body temperature to 35. 5-36 degrees can be observed, which is an extremely negative and dangerous symptom in any case, which should not be allowed.
In the middle stages of the disease, blood may be observed in the patient's urine. This sign is relatively rare and often not indicative, but extremely dangerous. It can begin to manifest itself due to purulent fusion of the prostate, trauma to the prostate gland, and also in cases of complications of the inflammatory process with hyperplasia. The cure in this case is complicated (often surgical intervention is necessary).
Treatment should begin immediately after the first symptoms of the disease appear. If there have been at least some, albeit insignificant, as it seems, problems with urination, which in some cases are accompanied by fever and pain in the area of simplicity, then you should immediately make an appointment with a urologist to clarify the diagnosis. It is imperative to pay attention to the signs of pathology described above, since it is possible to defeat prostatitis quickly and painlessly only with timely treatment.
Why does the prostate gland become inflamed?
Basically there are 2 main reasons:
- Infection. Most often, prostatitis develops precisely because of infection in the prostate. Infection can occur through the bladder, urethra, rectum, blood and lymph. It turns out that often prostatitis itself is a complication of an existing disease. Therefore, never self-medicate, you must first cure the source of the infection. Cystitis, pyelonephritis, urethritis, STIs (sexually transmitted infections) - this is understandable, they are directly related to the prostate. Even untreated tonsillitis, sinusitis, flu, caries can also come back to haunt the inflammation of the prostate.
- Circulatory disorders. This may be due to structural features, and due to spasms of the urethra, disorders of nerve conduction and the work of the muscles of the abdomen and pelvis, and also due to external factors.
However, whether prostatitis develops or not depends, first of all, on predisposing factors:
- Chaotic sex life. The abundance of sexual partners, especially unprotected contacts - this depletes the immune system, which must constantly face foreign microflora in female secretions. And sooner or later it fails.
- Long abstinence. This is the other extreme. The lack of sex has a bad effect on the general condition of a man, and especially on the prostate. Its secret stagnates, blood circulation is disturbed, an infection develops.
- Masturbation. It happens that men try to escape from the lack of sex by masturbation. However, this causes a decrease in the tone of the prostate, it becomes lethargic. It is even isolated into a separate type of prostatitis - congestive.
- Excess weight. In overweight men, the load on the pelvic organs is greatly increased, as well as on the whole body in general. The blood supply is disturbed, because of this, prostatitis, and hemorrhoids, and a host of other diseases occur.
- Hypothermia. "Don’t sit in the cold, " they say to all the girls. However, this also applies to men. At risk are lovers of extreme winter entertainment, avid fishermen, owners of old cars (oh, how often I see men lying on cardboard under the car in winter), even passengers on icy trains, as well as fashionistas with rolled up pants and no hat. Oh yes, and urinating outside in the winter is also fraught with serious consequences.
- Inactivity. Basically, this applies to the workflow, when you have to sit in one place for a long time: drivers, office workers. It is especially harmful to cross your legs, as the load on the prostate only increases.
- Stress. Psychological problems, chronic lack of sleep, an overloaded work schedule are the favorites of infections.
- Restraining the urge to urinate. Are the 5 minutes saved in a busy workflow worth the potential problems?
- Bad habits. Well, where without them? Abuse of alcohol and nicotine that only violate.
- Wrong nutrition. Fatty, spicy, salty foods are a magnet for diseases of the pelvic organs.
- background diseases. Any untreated infectious diseases can be complicated by prostatitis.
- Tight underwear. As well as "fashionable" overly tight trousers. They squeeze the small pelvis, disrupt blood circulation, cause swelling and inflammation.
- Physical overload. Professional athletes, loaders, active visitors to gyms are at great risk.
- Self-treatment. Sometimes men are ashamed to admit their problems even to a doctor, they try to crush the disease with various folk remedies, proven and not so good. However, it happens that without medicines prescribed by a competent doctor, one cannot cope here.

How is the disease diagnosed?
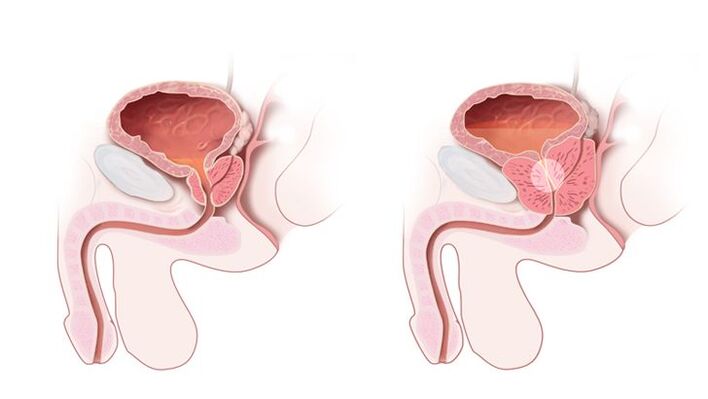
The diagnosis is established by a urologist or andrologistafter examining the patient, collecting an anamnesis and studying symptoms. The doctor needs to find out the patient's method of contraception, the presence of STIs in the sexual partner, the possibility of anal intercourse without a condom. This data facilitates the diagnosis and guides the physician's thinking in the right direction. The prescription of the onset of symptoms of the disease or discomfort in the perineum allows us to judge the course of prostatitis and its severity. The urologist necessarily examines the patient's genitals and conducts a rectal examination of the prostate gland. To do this, he inserts one finger into the anus of the patient and gropes on the anterior wall of the rectum protruding prostate. Soreness and its size indicate the intensity of the inflammatory process.
Next, the doctor conducts a series of instrumental, microscopic, bacteriological and immunological studies in order to clarify the cause of the disease. The most common diagnostic method is a 4- or 3-glass urine sample. The first method is more time-consuming and difficult to implement in practice, as it requires the patient to deliberately interrupt urination several times. The second modification is simpler: the patient continuously urinates into three different containers in equal portions. The first portion speaks about the state of the urinary tract, the second about the pathology of the bladder and kidneys, from the third they receive information about the state of the prostate gland. All collected material is examined under a microscope. With prostatitis, white blood cells and sometimes bacteria are found in the third portion of urine.
For microscopy, the secret of the prostate gland is also taken.To do this, the doctor performs a massage of the prostate through the wall of the rectum for some time so that it is emptied into the urethra. Smears are made from the collected material in the laboratory, stained and studied under high magnification. A sign of inflammation is leukocytes, bacterial etiology of the disease - bacteria in a smear. To determine the type of pathogen, the prostatic secret is sown on nutrient media. If pathogenic microorganisms are present in it, then after 3-5 days they form microbial colonies, which can then be studied. The bacteriological method allows obtaining data on the sensitivity of microflora to antibiotics.
Of the instrumental diagnostic methods are carried out:
- Ultrasound of the kidneys;
- TRUS of the prostate with dopplerography - an ultrasound probe is inserted into the rectum for the best visualization of the prostate gland, its blood flow is additionally assessed;
- Ascending urorethrography is necessary for persistent recurrent prostatitis. A radiopaque substance is injected into the urethra, after which a series of consecutive images are taken.
In addition to these methods, all types of research on STIs are of great importance. Among them are:
- PCR ejaculate, prostate secretion, scraping from the urethral mucosa - the method allows you to detect a wide range of pathogens;
- Blood ELISA - to detect specific antibodies to STI pathogens.
Types of prostatitis
In accordance with the criteria of the American National Institute of Health (NIH USA) from 1995, there are four categories of prostatitis:
- Category I: Acute prostatitis;
- Category II: Chronic bacterial prostatitis;
- Category III: Chronic prostatitis/chronic pelvic pain syndrome (CP/CPPS);
- Category IIIa: Chronic prostatitis / chronic pelvic pain syndrome with signs of inflammation;
- Category IIIb: Chronic prostatitis / chronic pelvic pain syndrome without signs of inflammation;
- Category IV: Asymptomatic (asymptomatic) chronic prostatitis.
Occasionally, chronic granulomatous prostatitis, not mentioned in this classification, also occurs.
In turn, most experts distinguish between:
According to the course of the disease:
- acute prostatitis;
- chronic prostatitis;

Depending on the causes of the disease:
- bacterial prostatitis;
- non-bacterial prostatitis
In most cases (especially in men under 40), bacterial prostatitis is noted.
Based on this, there are:
- acute bacterial prostatitis;
- chronic bacterial prostatitis;
- chronic abacterial prostatitis.
Prevention
To prevent the occurrence of inflammation or recurrence of chronic pathology, you must follow these recommendations:
- Reduce the amount of alcohol consumed;
- Do sports regularly;
- Avoid hypothermia;
- Stop smoking;
- Avoid stressful situations;
- Treat inflammation in time - first of all, this applies to genital infections;
- Take a contrast shower;
- Avoid lifting heavy objects;
- Use barrier methods of contraception;
- Regularly have sex;
- Take vitamin preparations;
- Engage in strengthening immunity;
- Visit a urologist twice a year;
- Eat right and balanced.
Purpose of the prostate in the male body: what is it responsible for?
The prostate is an exocrine gland in the male body.
Iron belongs to the reproductive system and is responsible for the production of a number of specific substances:

- the main one is the secret (prostatic juice), which provides the necessary viscosity of the ejaculate and, accordingly, normal sperm motility. When the sperm is too thick, fertilization is difficult, and a woman simply cannot get pregnant from a seemingly healthy man;
- other components maintain the normal composition of sperm. These include biologically active substances, immunoglobulins, enzymes, vitamins, microelements, etc. The norms of these substances are individual, and it is the prostate that regulates their content.
Thus, she is responsible for the reproductive abilities of a man, for the opportunity to have a regular and full sexual life and have children. This is the main function of the gland, but there are others, no less important.

























